
The Power of Menthol: Why I...
VIEW >

Chiropractor’s Guide to Inc...
VIEW >

Not yet a Pro Portal member? Sign up here.
Chiropractors, Physical Therapists, Massage Therapists and other Hands-On Healthcare Professionals are an essential health and wellness resource for individuals of all ages. We partner closely with these professionals on helping people perform better and move ‘pain-free’.
Our topical pain relief products were specifically formulated with these hands-on healthcare professionals (and their patients) in mind. Our fast-acting formulation with penetration enhancers plus 10% menthol, MSM, Glucosamine is like no other. Embracing hands-on healthcare professionals and topical pain relief solutions like Stopain® Clinical provides patients and their families with the ultimate wellness solution.
Visit our clinic locator to find a healthcare professional in your community.
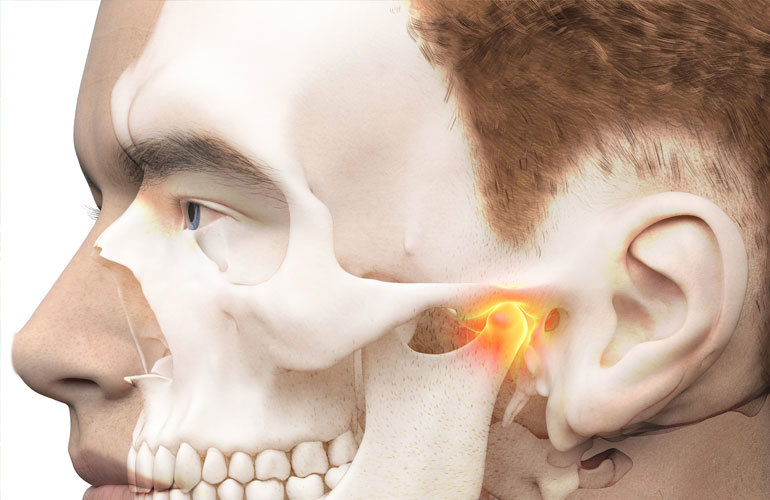
Temporomandibular disorders (TMD) is a broad term used to describe pain and dysfunction in the temporomandibular joint, face, head and neck. It has been associated with tinnitus, dizziness, fatigue and emotional stress with an estimated prevalence of 75% of the general population being affected at one time or another. The exciting news is that the current research supports a multimodal, conservative approach in the treatment of TMD, including CMT of the cervical spine.
Assessment begins with a history and examination. If you are the first clinician to evaluate the sudden onset of sharp, excruciating facial pain in the trigeminal region immediate referral is needed. Once TMD is suspected, exam findings will indicate the primary driver of the pain/dysfunction as either joint (arthrogenic), soft tissue (myogenic) or nerve (neurogenic) related. Often more than one variable is involved.
Relevant Tip: In the treatment of TMD joint dysfunction is often secondary to soft tissue and nerve involvement. Therefore, once the myogenic and neurogenic factors are alleviated the arthrogenic involvement often resolves.
Active and passive motion is assessed for pain, quality and quantity of motion - always on the lookout for noises. Active opening is expected to be at a ratio of 4:1 to lateral deviation and lateral deviation restricted by more than 5mm to one side indicates intra-articular TMJ dysfunction. Palpation of the TMJ for localized tenderness is an additional arthrogenic indicator. Patients with bruxing, clenching, and grinding often need dental appliances as does the patient that does not “hold” their treatments. Having a dentist on your referral team is necessary to treat TMD patients.
Relevant Tip: Consider mandible motion as a bilateral hinge joint and both sides need to be assessed and treated individually. For example, one side may be classified as arthrogenic and the opposite may be myogenic.
Soft tissue palpation for the region involves the muscles of mastication as well as related head and neck muscles. Palpate for taut and tender fibers, myospasm, fibrosis and trigger points. Remember, SCM and upper trapezius trigger points can also refer pain into the jaw and face!
The mandibular branch of the trigeminal nerve innervates the primary muscles of mastication and has sensory innervation to the lower third of the face. It can become entrapped by the mastication muscles and may also be involved in trigeminal neuralgia. While palpating the region be attentive for provocation of nerve pain throughout its distribution.
Relevant Tip: Pain management for neurogenic sub classification patients includes photobiomodulation (PBM Therapy) and topicals without counterirritants. Homeopathic and transdermal topicals are excellent choices. Application of topicals to the suboccipital and upper cervical regions can desensitize the C2 and C3 posterior rami which communicate with the Trigeminal Nerve nucleus. Therefore, the appropriate use of Stopain® Clinical Migraine & Headache over the suboccipital and cervical regions can have a significant impact in headache and TMD.
Manual trigger point release, active / passive myofascial release, IASTM, dry needling, and modalities such as ultrasound, TECAR, and PBM are excellent for treatment of myogenic syndromes. Neurogenic classification responds well to topicals, PBM Therpy, TECAR, and cognitive behavioral treatment. Arthrogenic syndromes favor topicals, CMT (spine and TMJ), soft tissue release, ultrasound and therapeutic exercises.
Headache, face and neck pain are common symptoms that present to our offices. Once assessed, set up a treatment plan to include modalities, soft tissue work and CMT in conjunction with the appropriate topicals such as Stopain® Clinical Migraine & Headache.
---
Dr. Donald DeFabio is in private practice in Berkeley Heights where he hosts seminars on a multi modal approach to Chiropractic as well as a CCSP to Rehab Diplomate program. His exercise protocols can be found on his You Tube Channel that has over 37K subscribers. For more information or to subscribe to his rehab tips newsletter visit www.DeFabioDifference.com
References: